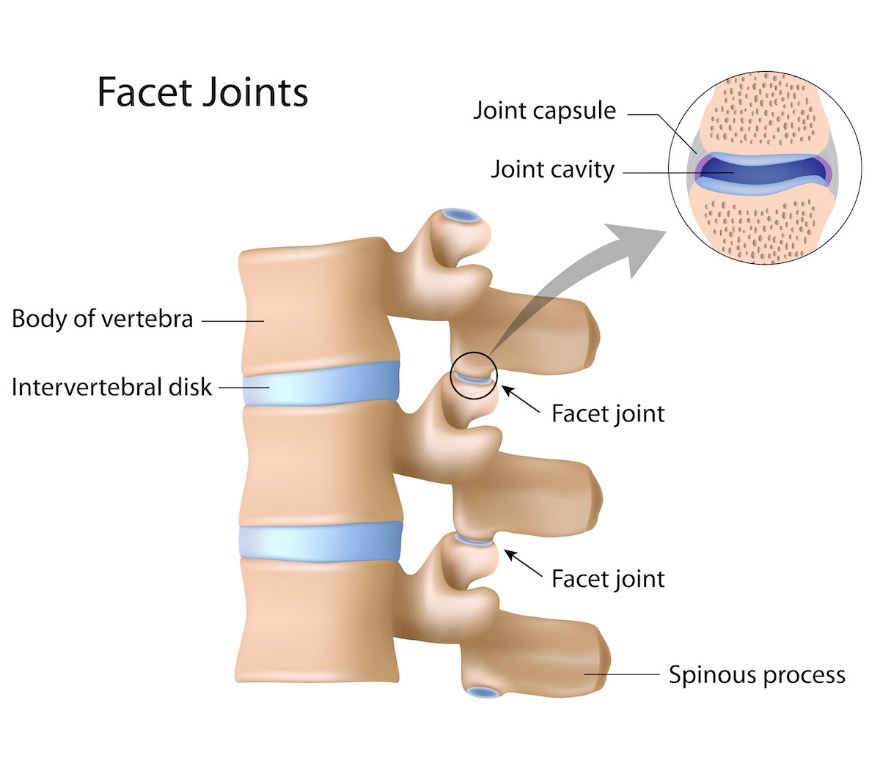
There are many causes as to why people get lower back pain. One common reason is the facet joint. The Journal of Spine Disorders and Techniques, define the joint as forming the superior and inferior articular process of two adjacent vertebrae. The function of the joint is to allow flexion and extension of the spine and to limit rotation. The joint also plays a crucial role in preventing the vertebrae from slipping over each other.
Facet joint disease or facet syndrome
Pain caused by the facet joint, often called facet joint disease or facet syndrome, is a condition where these joints become a source of pain. The journal Spine reported last year in Australia the prevalence of pain from the facet joint was 54%. The journal concluded that such is a common source of disability, with a significant economic impact. The journal Seminars in Arthritis and Rheumatism last year concluded that 89% of patients in the 60 to 69-year age group, have facet joint osteoarthritis, importantly not everyone was symptomatic.
A diagnosis, often by an experienced sports physiotherapist, needs to be made based on the history and the duration of symptoms, clinical assessment and clinical experience of other similar cases in the past. An in-depth clinical assessment is required, as there are several differential diagnoses that needs to be excluded. These can include sciatica, hip osteoarthritis, sacroiliac joint dysfunction, stress fractures, disc herniation, rheumatoid arthritis and many more.
Often the direction that a person prefers to move their spine, and not move, can be an indicator that the facet joint is a source of the symptoms. In not all cases, the pain is often described by patients as worse in the mornings, immediately after awakening, or during periods of inactivity. Sometimes a scan might be indicated, but not in the absence of a thorough clinical assessment. Often too much emphasis is placed on the scan, whereby a scan should be the last ‘tool’ in the ‘toolbox’, not the first.
Treatment options for the facet joint
In some cases, a ‘pain provocation injection’ or a ‘diagnostic block’ is used in conjunction with the clinical examination to identify if the facet joint is the cause of the pain. If the clinical assessment suggests that the source could be coming from a different structure, a provocative discography (positive if there is a change in pain, indicating that the disc is the source of symptoms), or a sacroiliac joint block (suggesting the sacroiliac joint is the source of symptoms) may be indicated.
It is important to realise that management varies with the particular presentations, so not every treatment plan is the same. After a diagnosis is made, conservative management is the first step in the process of treating facet joint pain. Some include strengthening and general exercises, physiotherapy, anti-inflammatory medications, weight loss, and massage.
When conservative measures fail, injections into the facet joint or radiofrequency ablation (or rhizotomy) can be performed. Radiofrequency ablation uses heat to temporarily destroy the sensory nerve, often resulting in a reduction of pain.
The last resort is surgery, but this certainly does not guarantee a positive outcome all the time.
One needs to consider the big picture, and how the lower back pain is affecting your quality of life.
Robert Vander Kraats is a sports physiotherapist with 18 years of experience, book in with him at Greenwood on 9203 7771 or online for your comprehensive assessment, and learn of any contributing factors.